42 medicare appeal process diagram
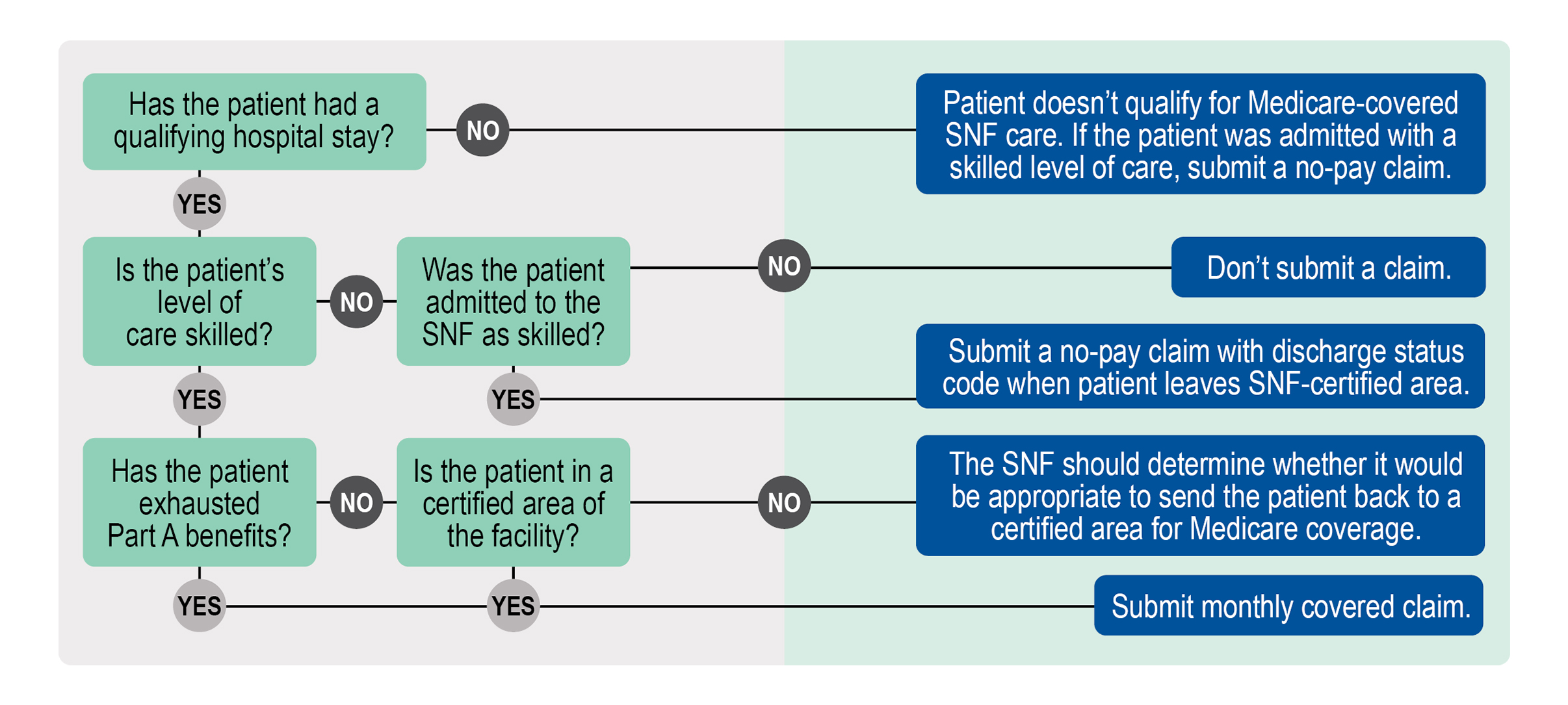
Appeal Process Skilled Services Appeals* Hospital Appeals Medical Record Requested and Received by Kepro Notice of Non-coverage Issued by Provider Important Message from Medicare Issued by Hospital Appeal Filed by Medicare Beneficiary or Representative Kepro’s Nurse and Physician Review the Medical Record Kepro’s Physician Makes a ... To see a diagram (flowchart) of the original Medicare (fee-for-service) standard and expedited appeals process, go to the "Downloads" section below. Appointment of Representative A party may appoint any individual, including an attorney, to act as his or her representative during the processing of a claim(s) and /or any claim appeals.
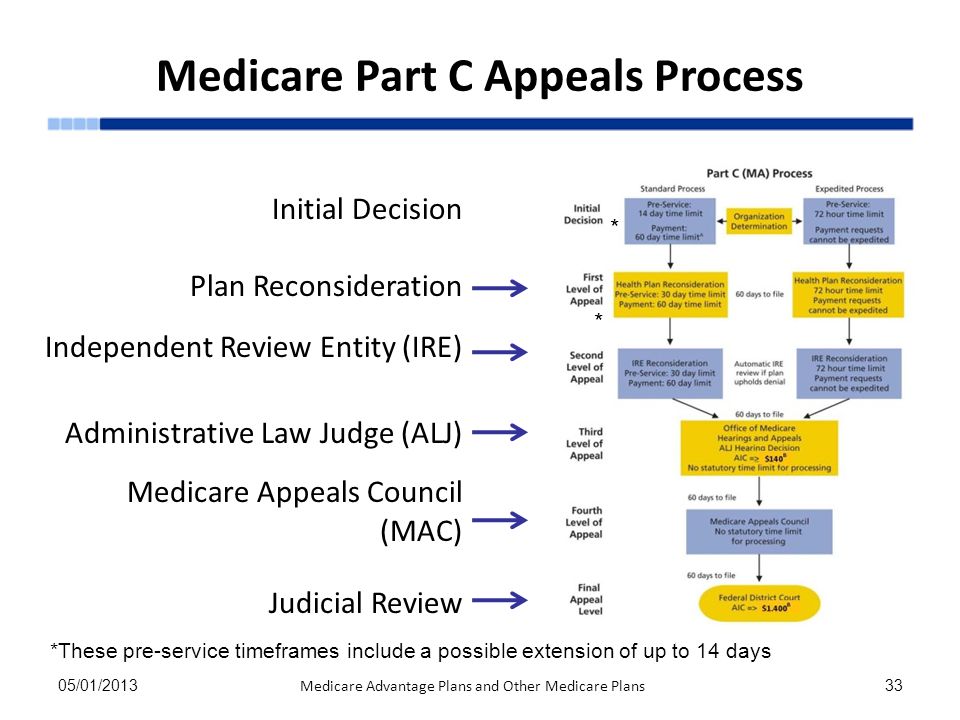
Level 3 is filing an appeal with the Administrative Law Judge (ALJ). ALJs hold hearings and issue decisions related to Medicare coverage determination that reach Level 3 of the Medicare claims appeal process. Level 4 is the Department Appeals Board (DAB) Review.

Medicare appeal process diagram
If you have a Medicare health plan, start the appeal process through your plan. Follow the directions in the plan's initial denial notice and plan materials. You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. Find more information on the CMS Appeals and Medicare Appeals webpages. Appealing Medicare Decisions. Medicare FFS has 5 appeal process levels:.17 pages How to file an appeal if your Medicare Advantage Plan doesn’t cover an item or service If you have a Medicare Advantage Plan, you know it covers a lot of items and services, like prescription drugs, diabetic test supplies, cardiovascular screenings, and hospital visits.
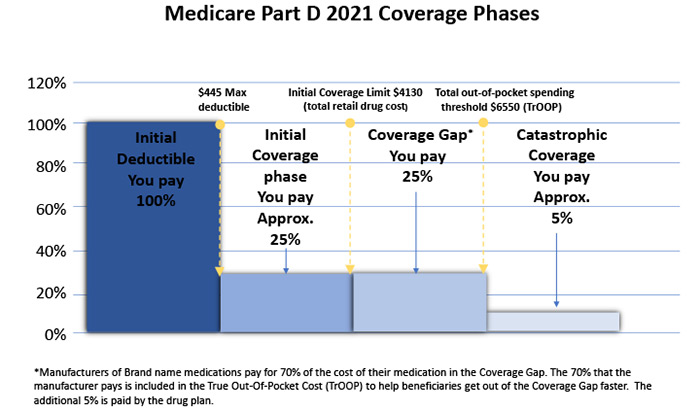
Medicare appeal process diagram. 25 Aug 2020 — Flowchart for Medicare Part D Appeals and Grievances ... DISCLAIMER: The contents of this database lack the force and effect of law, except as ... Coverage Determination*/Appeals Process. STANDARD PROCESS ... Office of Medicare Hearings and Appeals ... The chart reflects the amounts for calendar year 2021.1 page AIC = Amount In Controversy. ALJ = Administrative Law Judge. MAC = Medicare Administrative Contractor. *The AIC requirement for an ALJ hearing and Federal ...1 page 27 Jul 2018 — Once an initial claim determination is made, beneficiaries, providers, and suppliers have the right to appeal Medicare coverage and payment ...
New appeal rights are not triggered by a refusal to reopen, and appeal filing timeframes on the original initial determination are not extended following a contractor’s refusal to reopen. See, Pub 100-04 Medicare Claims Processing Manual, chapter 1, §70.5 for the distinction between Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan. File an appeal. How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan. Medicare Hearin gs and A ppeals ALJ Hearing AIC ≥ $180** No statutory time limit for processing . Medicare Appeals Council . No statutory time limit for processing . F. ederal District Court AIC ≥ $ Review1,760** First Appeal . Level Second Appeal Level Third Appeal Level Fourth Appeal Level Judicial Medicare Parts A & B Appeals Process MLN Booklet Page 6 of 17 MLN006562 May 2021. Appointing a Representative. A party may appoint an individual, including an attorney, at any time to represent them during the claim or appeal process. To appoint a representative, the party and representative must complete the .
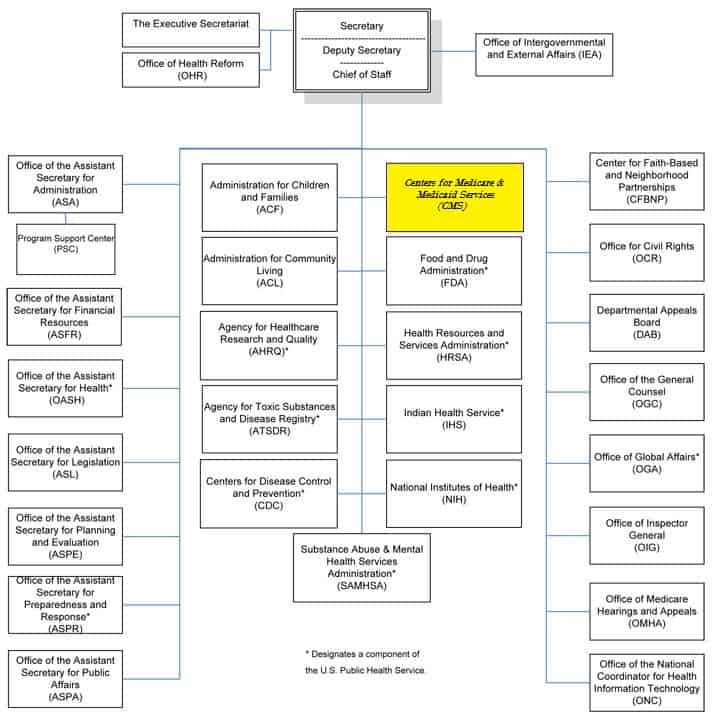
Medicare health plans, which include Medicare Advantage (MA) plans – such as Health Maintenance Organizations, Preferred Provider Organizations, Medical Savings Account plans and Private Fee-For-Service plans – Cost Plans and Health Care Prepayment Plans, must meet the requirements for grievance and appeals processing under Subpart M of the Medicare Advantage regulations. How to file an appeal if your Medicare Advantage Plan doesn’t cover an item or service If you have a Medicare Advantage Plan, you know it covers a lot of items and services, like prescription drugs, diabetic test supplies, cardiovascular screenings, and hospital visits. Find more information on the CMS Appeals and Medicare Appeals webpages. Appealing Medicare Decisions. Medicare FFS has 5 appeal process levels:.17 pages If you have a Medicare health plan, start the appeal process through your plan. Follow the directions in the plan's initial denial notice and plan materials. You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination.

Palmetto Gba Jm Home Health And Hospice Provider Contact Center Pcc Frequently Asked Questions Faq April 1 2020 June 30 2020

Revenue Cycle Management Process Flow Revenuecyclemanagement Healthcarerevenuecyclema Revenue Cycle Management Revenue Cycle Health Information Management

















0 Response to "42 medicare appeal process diagram"
Post a Comment